|
 |
|
|
What Are the Key Challenges Facing India’s Healthcare System Today?
India’s healthcare system, while having made considerable strides over the years, continues to face a range of complex challenges. These issues are deeply rooted in the country’s socio-economic fabric, geographic diversity, and population size. As a result, millions of Indians still lack access to adequate healthcare services. In this three-part exploration, we delve into the critical challenges facing India’s healthcare system today and examine potential paths forward. Inadequate Infrastructure and Urban-Rural Disparities1. Inadequate InfrastructureIndia’s healthcare infrastructure is critically under-resourced, making it difficult to meet the needs of its 1.4 billion people. Shortage of Beds:
With less than 1.4 hospital beds per 1,000 people, India falls well below the World Health Organization’s (WHO) recommended ratio of 3.5 beds per 1,000. This shortage is especially pronounced in public hospitals, which often see overcrowding and long wait times. While the private sector has over 1.18 million beds, the public sector lags behind with just 713,986 beds, leading to a disparity in access to care. Underfunded Public Facilities:
Government healthcare spending in India is less than 2% of the country’s GDP, significantly lower than that of many other nations. This chronic underfunding has resulted in outdated infrastructure, a lack of advanced medical equipment, and insufficient resources to handle growing patient demands. For instance, many public hospitals lack diagnostic tools, leading to delayed or inaccurate treatment. Impact of COVID-19:
The pandemic further exposed the fragility of India’s healthcare infrastructure, with hospitals struggling to cope with surges in cases. Temporary field hospitals and increased private sector involvement offered some relief, but these measures underscored the urgent need for permanent improvements in healthcare facilities.
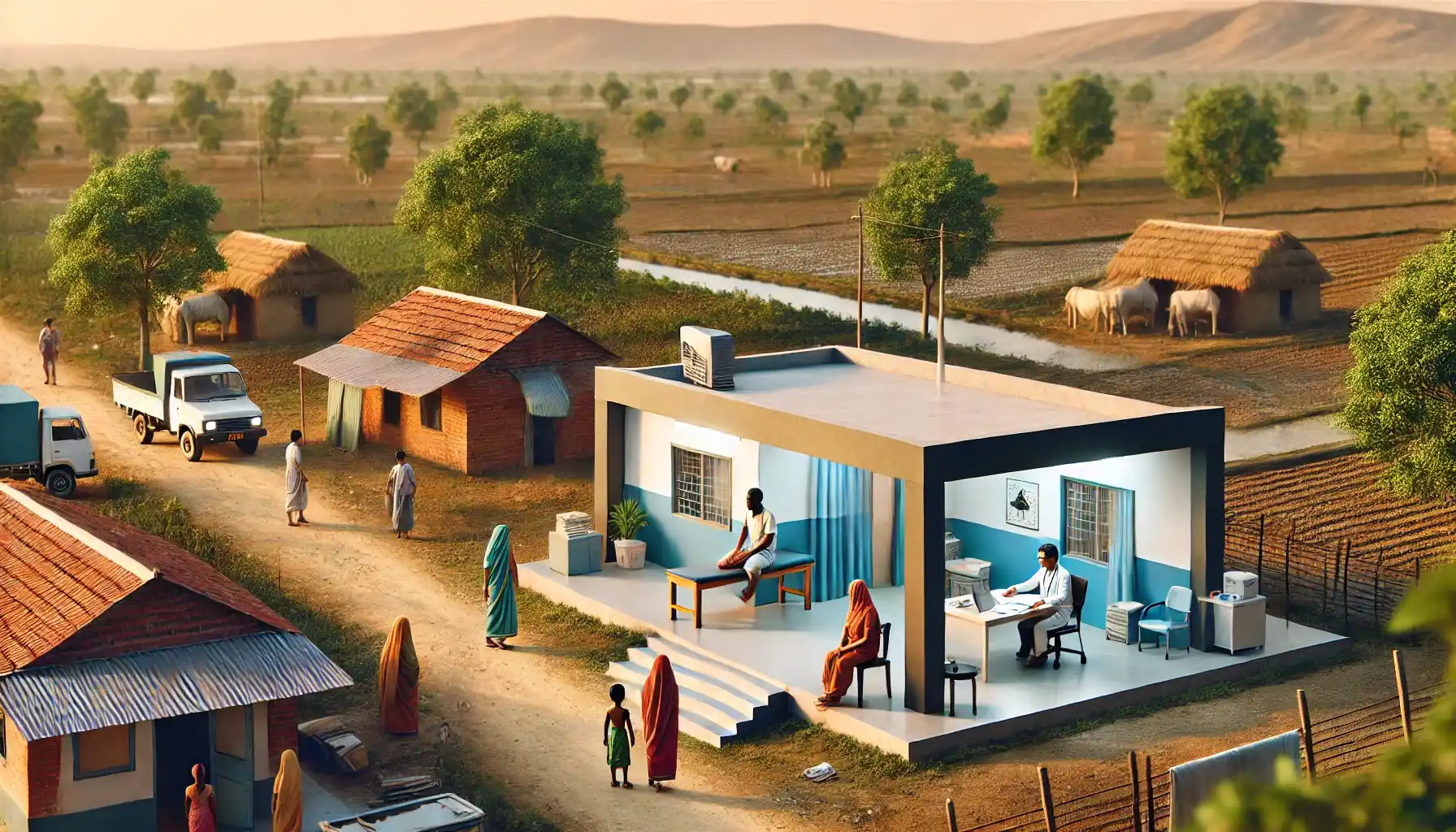
2. Urban-Rural DisparitiesIndia’s urban-rural divide creates a stark contrast in healthcare accessibility and outcomes. Better Facilities in Urban Centers:
Cities typically enjoy better-equipped hospitals, specialized care, and easier access to advanced treatments. This concentration of resources in urban areas leaves rural regions underserved, where nearly 65% of India’s population resides. Rural hospitals and clinics often lack basic necessities such as running water, electricity, and qualified medical personnel. Shortage of Specialists:
While urban hospitals may have multiple specialists on hand, rural health centers struggle to retain doctors, nurses, and other healthcare workers. Many rural clinics are staffed by just one or two professionals, limiting the scope of services they can provide. Poor Transportation and Connectivity:
Geographic isolation further exacerbates healthcare access in rural areas. Poor roads and inadequate public transportation make it challenging for patients to travel to distant hospitals, delaying critical care. This issue is especially pressing during emergencies, where every second counts.
Consequences of Infrastructure Gaps and Urban-Rural DivideThese inadequacies disproportionately impact vulnerable populations, including the elderly, women, and children in rural areas. For example, rural maternal mortality rates remain significantly higher than in urban centers due to a lack of access to prenatal and emergency care. Similarly, rural patients with chronic conditions such as diabetes or hypertension often go undiagnosed or untreated, worsening their health outcomes. What’s Needed to Bridge the Gap?Addressing these challenges requires a multi-faceted approach: Increased Public Investment:
The government must prioritize healthcare spending to build more hospitals, upgrade existing facilities, and invest in advanced medical technology. Public-private partnerships could play a crucial role in accelerating infrastructure development. Decentralized Healthcare Delivery:
Decentralizing healthcare services can bring medical care closer to rural communities. Mobile clinics and telemedicine initiatives, supported by improved internet connectivity, can make quality healthcare more accessible in remote areas. Incentives for Rural Healthcare Workers:
Offering better compensation, housing, and career growth opportunities can attract more healthcare professionals to rural areas. Training programs for community health workers can also fill gaps in primary care.
3. Shortage of Healthcare ProfessionalsIndia’s healthcare system is critically short-staffed, with an insufficient number of doctors, nurses, and specialists to meet the growing demands of its population. Low Doctor-to-Patient Ratio:
The WHO recommends a doctor-to-patient ratio of 1:1,000, but India’s ratio stands at approximately 0.8:1,000. This shortage is even more severe in rural areas, where healthcare facilities often operate without a single full-time doctor. Nurse and Paramedic Deficit:
Nurses and paramedics form the backbone of any healthcare system, yet India faces a significant deficit in these professions. With an average of 1.7 nurses per 1,000 people (compared to the global standard of 3 per 1,000), many healthcare facilities struggle to provide adequate care. Specialist Gap:
Critical fields such as cardiology, oncology, and pediatrics suffer from a lack of trained professionals. This gap forces patients to travel long distances to urban centers for specialized treatments, delaying care and increasing costs. Brain Drain:
India also faces the challenge of losing skilled healthcare professionals to countries offering better salaries, infrastructure, and working conditions. This phenomenon, known as “brain drain,” further exacerbates the shortage.
Consequences of Workforce ShortagesThe lack of healthcare professionals leads to: Longer wait times for patients, often stretching into months for specialist consultations. Burnout among existing staff due to excessive workloads. Compromised quality of care, with overburdened professionals unable to dedicate sufficient time to individual patients.
Potential SolutionsExpand Medical Education:
Increasing the number of medical colleges and nursing schools, particularly in underserved areas, can help train more healthcare professionals. Subsidized education and scholarships for students from rural backgrounds can encourage them to serve in their communities. Task-Shifting:
Training community health workers and paramedics to handle basic medical tasks can alleviate the burden on doctors and nurses. These workers can provide primary care and preventive services in rural areas. Improve Working Conditions:
Competitive salaries, better infrastructure, and career development opportunities can reduce brain drain and attract skilled professionals to underserved regions.
4. High Out-of-Pocket ExpenditureIndia’s healthcare system relies heavily on out-of-pocket payments, with patients bearing nearly 75% of total healthcare costs. This financial burden can deter individuals from seeking timely medical care or lead to catastrophic health expenditures that push families into poverty. The Cost of Care:
For many Indians, even basic healthcare services are unaffordable. Diagnostic tests, hospital stays, and medication costs often consume a significant portion of household income. Impact on Vulnerable Populations:
Low-income families and those without health insurance are disproportionately affected. For example, a single hospital admission for a major illness can deplete a family’s savings, forcing them to borrow money or sell assets to cover expenses. Medical Debt:
High out-of-pocket costs lead to mounting medical debt, which can trap families in a cycle of financial instability. In rural areas, this issue is compounded by the lack of affordable healthcare facilities, forcing patients to seek expensive care in urban centers.
Limited Health Insurance CoverageWhile government initiatives like Ayushman Bharat aim to provide insurance coverage for low-income families, many Indians remain uninsured or underinsured. This leaves a significant portion of the population vulnerable to financial strain in the event of illness. Consequences of Financial BarriersDelayed or Skipped Treatment:
Fear of high medical bills often causes patients to delay or forgo necessary treatment, leading to worsening health conditions. Health Inequity:
Wealthier individuals can afford advanced treatments, while low-income groups struggle to access even basic care, widening the health disparity gap. Undermining Public Health Goals:
High out-of-pocket costs reduce participation in preventive health measures like vaccinations and regular check-ups, undermining efforts to control diseases.
Potential SolutionsExpand Insurance Coverage:
Government programs like Ayushman Bharat should be scaled up to cover more people and provide comprehensive benefits, including outpatient care and preventive services. Subsidize Essential Services:
Subsidizing the cost of diagnostic tests, medications, and hospital stays in public healthcare facilities can make healthcare more affordable for low-income families. Promote Public Awareness:
Educating people about existing insurance schemes and financial assistance programs can help them access benefits and reduce out-of-pocket expenses. Strengthen Public-Private Partnerships:
Collaborations between the public and private sectors can increase the availability of affordable healthcare services, particularly in rural areas.
5. Fragmented Healthcare SystemIndia’s healthcare system is characterized by a mix of public and private providers, which operate independently and often lack coordination. This fragmentation leads to inconsistencies in the quality of care and creates confusion for patients. Public vs. Private Divide:
Public healthcare services are often underfunded and overcrowded, while private facilities, though better equipped, are unaffordable for a large segment of the population. This dual system creates a stark divide, with the wealthy accessing high-quality private care and the poor relying on overstretched public facilities. Varying Standards of Care:
Quality of care varies significantly across providers, with some private clinics operating without proper accreditation or oversight. Patients frequently face difficulties in evaluating the reliability of healthcare services. Lack of Integrated Systems:
The absence of a unified health information system prevents the seamless sharing of patient records between providers. This results in fragmented care, repeated diagnostic tests, and a lack of continuity in treatment.
Consequences of FragmentationInefficient Resource Allocation:
Limited collaboration between public and private sectors leads to duplication of services in some areas and shortages in others. Patient Confusion:
Patients often struggle to navigate the healthcare system, leading to delays in seeking care and higher costs. Inconsistent Outcomes:
Variations in care quality result in unequal health outcomes, with some patients receiving world-class treatment and others facing substandard care.
Potential SolutionsStrengthen Regulation:
Establishing robust regulatory frameworks for both public and private providers can ensure consistent quality standards. Promote Public-Private Partnerships:
Encouraging collaboration between sectors can optimize resource use, expand access, and improve service delivery. Create a Unified Health Information System:
A centralized system for storing and sharing patient records can improve care coordination and reduce redundancies.
6. The Burden of Non-Communicable Diseases (NCDs)India is experiencing a rapid rise in non-communicable diseases (NCDs) such as diabetes, hypertension, and cardiovascular conditions. These illnesses now account for over 60% of deaths in the country, adding to the existing burden of communicable diseases like tuberculosis and malaria. Consequences of NCDsIncreased Healthcare Costs:
Managing chronic diseases requires ongoing treatment and medication, significantly raising healthcare expenditures. Loss of Productivity:
NCDs often affect working-age individuals, leading to decreased productivity and economic losses. Pressure on Resources:
The dual burden of communicable and non-communicable diseases overwhelms healthcare infrastructure and personnel.
Potential SolutionsStrengthen Primary Care:
Integrating NCD management into primary healthcare services can ensure early diagnosis and treatment. Promote Health Education:
Public awareness campaigns about the importance of regular check-ups, healthy diets, and exercise can help reduce the prevalence of NCDs. Invest in Screening Programs:
Large-scale screening initiatives can identify at-risk individuals and provide preventive care, reducing the overall disease burden.
7. Lack of Focus on Preventive HealthIndia’s healthcare system has traditionally emphasized curative care, often neglecting preventive measures that could reduce the overall disease burden. Limited Public Health Initiatives:
Vaccination programs, maternal health initiatives, and sanitation campaigns are often underfunded and poorly implemented. Neglect of Lifestyle Education:
Preventive health measures, such as promoting physical activity and reducing tobacco use, receive little attention in public health policies.
Consequences of Neglecting PreventionHigher Disease Burden:
Failure to prioritize preventive care increases the prevalence of avoidable diseases, placing additional strain on healthcare resources. Missed Opportunities for Cost Savings:
Preventing diseases through early intervention is far more cost-effective than treating advanced conditions. Poor Health Outcomes:
A lack of focus on prevention contributes to India’s high rates of maternal mortality, infant mortality, and malnutrition.
Potential SolutionsRebalance Healthcare Priorities:
Allocating more resources to preventive care can reduce long-term healthcare costs and improve population health. Expand Community Outreach Programs:
Initiatives that educate communities about hygiene, nutrition, and vaccinations can empower individuals to take charge of their health. Leverage Technology:
Mobile health apps and telemedicine platforms can disseminate preventive health information and reach underserved populations.
Conclusion: The Path ForwardIndia’s healthcare system faces numerous challenges, from infrastructure deficits and workforce shortages to rising NCDs and fragmented care. Addressing these issues requires a comprehensive, multi-pronged approach that prioritizes both systemic reforms and community-level interventions. Key Actions for Improvement: Increase Public Healthcare Investment: Greater funding for public health infrastructure and workforce training is essential. Enhance Policy Coordination: Integrating public and private sectors can create a more cohesive and efficient healthcare system. Promote Preventive Health: Shifting the focus toward prevention can significantly reduce the burden of disease and improve overall outcomes.
At Niramaya Clinic, we are committed to being part of the solution. By offering accessible, high-quality healthcare services and raising awareness about preventive care, we aim to contribute to a healthier and more equitable India. To learn more about our services and initiatives, visit Niramaya Clinic. Together, we can work toward a future where every Indian has access to the care they need.
|